What You Need to Know About Keratoconus

Keratoconus presents in almost 50 of every 100,000 Americans and one in every 2,000 people worldwide. Your day-to-day activities should be fine if you have keratoconus. While irritation and inflammation from allergies could worsen keratoconus, you can use prescription glasses or contact lenses to correct your sight.
Many wrongly believe eyeballs do not grow after birth, yet our eyes grow like the rest of the body. Only the eyes grow slower as compared to other body parts. Also, different parts of the eye grow at different paces. Therefore, it’s common for the cornea to grow slower and become thinner and out of shape.
What is Keratoconus?
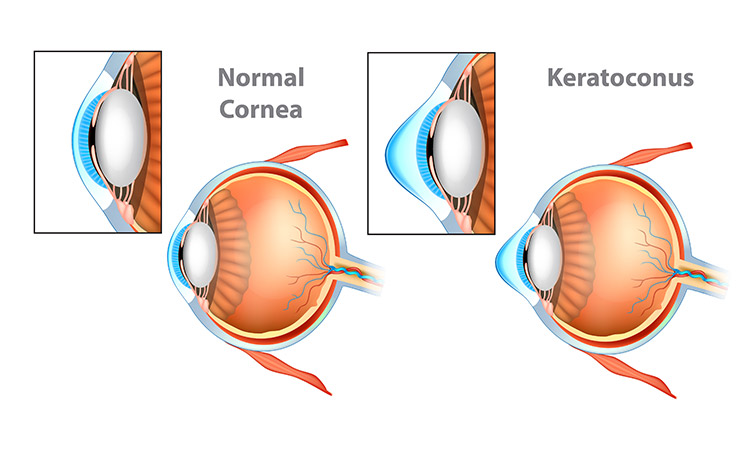
Keratoconus is a progressive disease that causes the cornea, the dome-shaped eye surface tissue, to thin and protrude outward into a conical shape. Typically, the cornea focuses incoming light onto the retina for clear vision. The cornea may sometimes become thin and weak and unable to maintain its round shape.
When this happens, the cornea bulges out, assuming a football shape, making it challenging to support clear vision. Vision blurring, sensitivity to light, and glare are all potential effects of a cornea with a cone shape. Typically, keratoconus affects both eyes, but one eye is often more affected than the other. It usually starts to impact people between the ages of 10 and 25.
For ten years or more, the condition may deteriorate steadily. Often, keratoconus results in high levels of astigmatism. When the tiny fibers of protein in your eyes can’t hold your cornea in place any more, you develop keratoconus. It occurs when you don’t have enough protective anti-oxidants in your cornea.
The corneal cells produce harmful byproducts, which the anti-oxidants remove to protect the collagen fibers. Sometimes, the anti-oxidant levels become too low, weakening the collagens and making the cornea protrude outside.
Your cornea is the outer lens of the eye. The dome-shaped eye surface acts as a windshield, and any interference might compromise your vision.
What Are the Symptoms of Keratoconus?
Keratoconus symptoms include:
- Blurry vision
- Astigmatism
- Increased sensitivity to light
- Frequent changes in glass or contact lenses prescription
- Difficulty with night driving
- Nearsightedness
Note that the symptoms may change as the disease progresses. Also, not all signs listed above point to keratoconus. Some may indicate deep-lying health conditions that need urgent medical attention. If you suspect you might be having keratoconus, make an appointment with your doctor for an eye exam. During the exam, your ophthalmologist will measure the size and shape of the cornea.
Causes of Keratoconus
There needs to be more research and information about the causes of keratoconus. So, the sources remain unknown, though many doctors point to genetically related factors. According to the National Institute of Health, Keratoconus results from a defect in collage, a vital tissue that makes up most of the cornea. Also, several studies have shown that around one in 10 people with keratoconus have a parent with the same condition.
Professionals in the eye care industry are still grappling with many theories about the cause of keratoconus. The approaches include enzyme imbalances and exposure to UV rays. Also, the doctors are trying to find a connection between excessive rubbing of the eyes and keratoconus. If you already have keratoconus, avoid rubbing your eyes.
The symptoms appear in teens and may continue to manifest throughout adulthood. Yet, the symptoms may appear earlier in some individuals.
Some of the risk factors associated with keratoconus include:
- Family history
- Excessive eye rubbing
- Allergies
How is Keratoconus Diagnosed?
Diagnosis of keratoconus begins with a review of your family and medical history. Additionally, your doctor may do more tests to determine the shape of your cornea. Your ophthalmologist may use an advanced diagnostic machine known as a topographer. The topographer reveals details such as the shape and thickness of the cornea. Your doctor will repeat the cornea measurement during each visit or check-up to help monitor your condition.
Some of the tests performed to diagnose keratoconus include:
- Eye refraction: Your doctor uses special equipment to check for eye problems. The doctor will use different methods to ascertain which lens combination may give your sharp vision.
- Slit-lamp examination: This method involves the usage of a low-powered microscope to evaluate the shape of your cornea and find out other potential eye disorders.
- Computerized corneal mapping, which produces a detailed map of your cornea. It also measures the thickness of your cornea.
Treatment of Keratoconus
There isn’t a one size fits all treatment for keratoconus. Your treatment depends on the extent of your condition and how fast the situation is worsening. While the symptoms might range from mild to severe, there are only two ways of managing or treating keratoconus. Depending on the nature of your condition, your doctor may slow down the disease’s progression or improve your vision.
If you have progressive keratoconus, your doctor may suggest corneal collagen cross-linking to slow or stop the progression. This treatment reduces the need to have a cornea transplant in the future. The therapy might slow down the progression of keratoconus but doesn’t reverse the disease or improve your vision. Cross-linking cannot restore your lost vision but may prevent future vision impairment.
Mild cases of keratoconus might need contact lenses or prescription glasses. Eyeglasses might be a long-term treatment if your cornea becomes stable later. Also, you might only use glasses when first diagnosed with keratoconus. Glasses might not be viable if the condition progresses and becomes more severe.
Cornea transplant surgery might be necessary for extreme conditions where the cornea becomes scarred.
Takeaway
Keratoconus starts in adolescence and gradually worsens as the patients approach their 20s. The disorder varies in every individual, and many options exist to correct keratoconus. Consult an ophthalmologist because only one can correctly interpret the corneal imaging studies and recommend a suitable treatment method. Discuss with them your preferred options.