Diabetic Retinopathy: Stages and Treatment
Diabetic retinopathy is one of the significant causes of visual impairments in patients between 25 and 74 years. Yet, early diagnosis and treatment can prevent its progression.
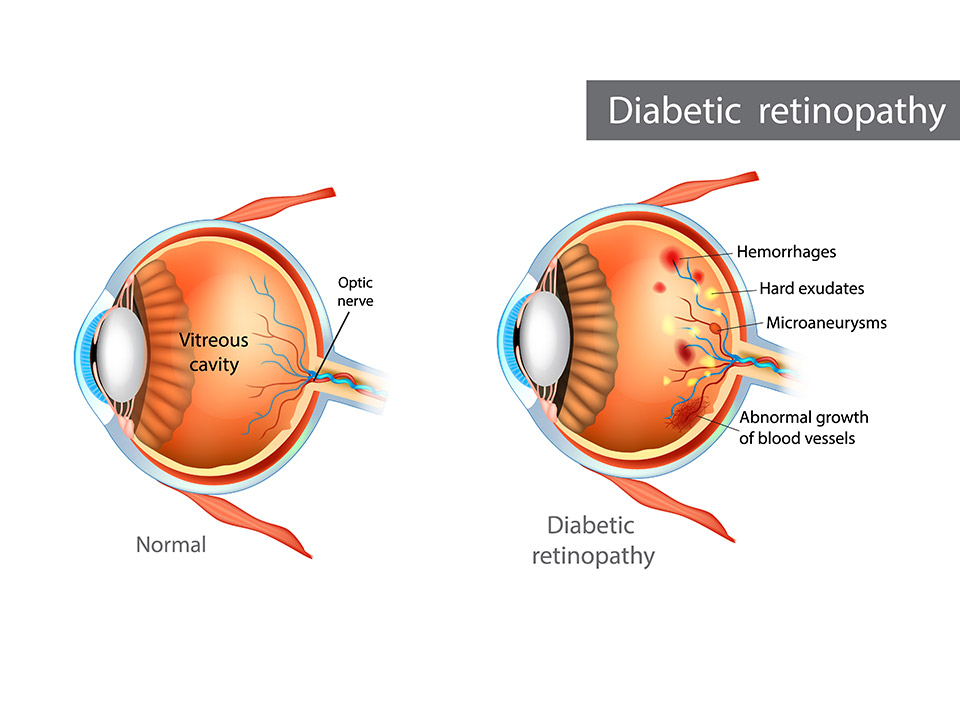
Diabetic retinopathy is a condition that arises when excessive blood sugar damages the tiny blood vessels in the retina. You can only see clear images when light rays come into focus on the retina. People who have diabetes are at an increased risk of developing neurovascular disorders, a complication that causes diabetic retinopathy.
Researchers say that diabetic patients are likely to develop diabetic retinopathy five years after being diagnosed with diabetes. If you go to the hospital with diabetic symptoms, your doctor will likely recommend eye impairment tests. High blood sugar is just as dangerous to your cardiovascular system as to the eyes.
It’s also possible to treat diabetic symptoms, yet the major problem is the destruction of the nerves within the retina. Therefore, it’s essential to have regular eye tests to detect any case of diabetic retinopathy.
What’s Diabetic Retinopathy?
Diabetic retinopathy is a disease that develops when high blood sugar destroys blood vessels in the retina. Damage to the retinal blood vessels leads to blurred vision. Severe cases of nerve impairment could lead to permanent vision loss.
Therefore, as a diabetic patient, you must undergo regular eye exams. Usually, the symptoms of diabetic retinopathy present after eye damage has already occurred.
How to Detect Diabetic Retinopathy?
If you have diabetic retinopathy, your weakened retinal capillaries may leak or rupture, causing hemorrhage/bleeding. Unfortunately, the symptoms don’t appear for many people until the disease progresses to an advanced stage.
As a patient, you must gather all the necessary information about the diabetic retinopathy condition. For instance, during the early stages, diabetic retinopathy doesn’t cause any noticeable symptoms. So, you may not notice you have the condition.
However, eye tests help a professional eye doctor to detect diabetic retinopathy in the early stages.
What Are the Stages of Diabetic Retinopathy?
Non-proliferative refers to the early stage of diabetic retinopathy, while proliferative is the advanced form of the disease.
Stage 1: Mild Non-proliferative Diabetic Retinopathy
Stage one is considered not so serious and may not need a referral to a retina specialist. Some clinical findings during this stage include tiny swellings in the retina’s blood vessels. The areas of swelling are likely to cause leakage in the retina, which eventually triggers swelling in the macula, the retina’s center.
However, these symptoms are usually never a cause for serious concern and may not show easily. Still, discussing exam findings with your doctor is crucial, especially if you have been diagnosed with diabetes. Fluid leakage in the retina could be an early sign of organ damage from diabetic diseases.
Stage 2: Moderate Non-proliferative Diabetic Retinopathy
Hemorrhages characterize this stage because the tiny retinal blood vessels swell up to block blood flow. Vision will be severely compromised when the retina lacks adequate blood supply and nourishment. Again, this stage has few visible symptoms; you will only notice signs if blood accumulates in the macula.
Remember, the doctor needs to discuss with the patients their findings and what they think about the diseases and the symptoms. The doctor may suggest treatment methods depending on the patient’s blood sugar levels and the last diabetes examination.
Stage 3: Severe Non-proliferative Diabetic Retinopathy
Massive blockage of blood vessels in the retina characterizes stage three. Typically, any blockage causes insufficient blood flow into the retina. When the retina doesn’t receive enough blood, it sends a signal to the body. The signals trigger the body to start growing new blood vessels.
The new blood vessel doesn’t help much because most are always thin and weak, causing excessive retina swelling. Sometimes, these new vessels leak into the macula, which may cause unexpected permanent vision loss.
Stage 4: Proliferative Diabetic Retinopathy
At this stage, diabetic retinopathy patients need immediate attention from a retina specialist. The specialist should conduct comprehensive testing and further treatment. Proliferative is the most advanced stage of diabetic retinopathy, where new blood vessels continue to grow in the retina.
Most of these new blood vessels are thin and weak and prone to excessive bleeding, causing scar tissue inside the eye. The scar tissue formed might pull your retina from its normal position, resulting in retinal detachment. You may experience symptoms like blurry vision, a narrowed field of vision, and even irreversible blindness if you have a detached retina.
Treatment
Not all types of diabetic retinopathy may require treatment. However, if the condition has affected the macula or abnormal new blood vessels begin to appear, you may need urgent treatment.
Unfortunately, there is no definite cure for diabetic retinopathy. However, several treatments may work well to prevent the condition from worsening, delaying, or reducing vision loss. Again, treatment is only easy if you detect the condition early.
Diabetic retinopathy needs you always to keep your sugar levels in control. Blood sugar control is one way to prevent the condition from worsening.
Treatment options include:
Laser Treatment
Laser treatment may only be effective if the retina is unaffected. You can use it to prevent vision loss. In severe proliferative retinopathy, you may need a more invasive laser therapy known as the scatter. The procedure reduces the growth of new blood vessels at the back of your retina.
Surgical Removal of The Vitreous Gel
If severe scar tissues have formed in the eye, your doctor might suggest surgical removal of the vitreous gel. This procedure works well only in cases where the retina isn’t severely damaged.
Anti-VEGF or Anti-inflammatory Medicine
Anti-VEGF medicines slow the unwanted growth of abnormal blood vessels in the retina. Using anti-VEGF medicines will slow down the growth of such vessels.
Takeaway
Diabetic retinopathy is a severe progressive eye disease that can lead to permanent vision loss. As a diabetic patient, you need regular eye exams to identify retinopathy before it worsens. Thus, an early diagnosis and treatment are the best way to prevent vision loss and other vision impairments.




