5 Vision-Related Problems That Diabetes Can Cause
You can prevent diabetes vision-related problems by having an early diagnosis.
Did you know diabetes is the primary cause of blindness in adults aged 20 to 74, and over 30 million Americans have diabetes? According to the Centers for Disease Control, 90% of patients have Type 2 diabetes. The most tragic part is that nearly all these people don’t know they have diabetes. Diabetes slowly damages your eyes and eventually results in blindness.
However, you can manage the situation by getting an early diagnosis and going for regular eye check-ups. Patients with Type 2 diabetes can’t handle insulin well and maintain normal blood sugar levels. In most instances, diabetic patients visit an ophthalmologist for eye treatment only to be referred for a diabetes check-up.
This article discusses some vision-related problems that might develop without prompt diabetes treatment.
1. Glaucoma
Not all glaucoma cases are diabetes related. However, you are more likely to get rare neovascular glaucoma if you have diabetes. Glaucoma occurs when too much pressure builds in the eye. The pressure builds up because the eye fluid doesn’t drain, eventually destroying the optic nerves and blood vessels.
In some patients, the colored part of the eye (the iris) may develop some growth. The blood vessels in the growth prevent eye fluid from flowing out, thus increasing pressure. Different types of glaucoma affect the eye differently. Unfortunately, many of them don’t have easily noticeable symptoms, and thus patients often lose their vision even without noticing.
You can’t prevent glaucoma, but you can stop it from worsening. Some medications lower the amount of excess fluid in the eye. Also, eye drops and laser treatments can manage glaucoma. Your ophthalmologist can use a laser to reverse the formation of new blood vessels by reducing them in the back of the eye.
2. Blurry Vision
Loss of sharpness of vision may occur if you don’t wear the prescribed corrective lenses. However, blurred vision could also result from underlying issues such as diabetes mellitus. Blurry vision can be caused by both the short and long-term effects of diabetes.
A diabetic patient has high blood sugar or glucose levels. High blood sugar in the body causes the lens inside your eyes to swell. Swelling of the eyes affects your inability to see clearly, either temporarily or permanently.
In case of very low blood sugar in the body, you may experience temporary blurred episodes, which may resolve once glucose levels return to normal. When the lens in the eye swells, blood vessels swell and leak, compromising clear vision.
The more the lens of the eye swells, the more likely they are to change in shape. The lens focuses light onto the back of the eye. When it swells, it doesn’t correctly refract light.
We also have the retina, light-sensitive layer cells found at the back of the eye. The retina converts light entering the eye into electric signals. The brain then turns the electric signals into clear images. If the retina doesn’t get enough supply of blood, you may not be able to see clearly.
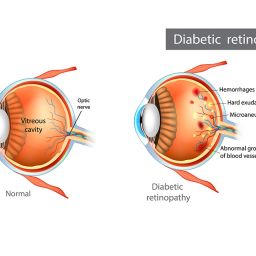
3. Diabetic Retinopathy
This diabetic condition majorly affects the eye’s retina. A retina is a group of cells that transform light into electric pulses. The pulses travel to the brain, where they convert into images you can see. High blood sugar levels can damage some of the most delicate blood vessels in the retina.
Most diabetic patients don’t show any symptoms of diabetic retinopathy until stage 4. Diabetic retinopathy is a common eye disease and a significant cause of blindness in adults. This condition damages blood vessels, making them swell and ultimately leak. However, some new abnormal blood vessels may develop and cause further vision problems.
If you have type 1 and type 2 diabetes and are pregnant, you will likely develop diabetic retinopathy. Also, patients who have had diabetes for a long time are at higher risk of getting diabetic retinopathy.
Diagnosis of diabetic retinopathy involves checking how well you can identify letters or symbols from a distance. Your ophthalmologist may examine the retina and inside of your eyes to determine any leaky blood vessels. If the diagnosis turns out positive, you will have to undergo an eye check-up at least twice a year. Patients with type 2 diabetes have the highest risk of developing diabetic retinopathy.
4. Macular edema
Diabetic patients have either too much or too low glucose levels. High sugar levels severely damage tiny blood vessels in the retina. The macula, the central part of the retina, is a critical part of the eye that sends images to the brain. Thus, the eye becomes adversely affected when high blood sugar levels damage blood vessels supplying the macula.
Macula edema (swelling) occurs during the early stages of diabetic retinopathy. The swelling of blood vessels and leakage into the macula causes the macula to swell. The oozing of blood from vessel walls causes swelling in the macula. Macula edema is a severe condition that can cause blindness if not managed early.
5. Cataract
The natural eye lens lets your eyes focus on an image and see clearly. If you have a camera, you will notice that sometimes the lens gets smoky or cloudy. So, you are unable to focus on an image properly. At times a cataract forms causing the eye lens to get cloudy.
Cataracts can affect anybody, but if you have diabetes, you are more likely to get it earlier than others. If left unchecked, cataracts can get worse faster. You may need surgery to remove the cloudy lens and replace it with an artificial one.
Takeaway
Diabetic patients have either high or low levels of sugar in the body. Excess sugar in your bloodstream can damage the blood vessels and nerves that run throughout the body, including the eyes. Regular check-ups, at least twice a year, can help identify problems early enough when they are easy to treat. Get dilated eye exams early to prevent vision loss from diabetes.